TL:DR – Thanks to GINA I have not needed to use salbutamol to treat my asthma for three years at the time of writing.
It’s three years since my asthma nurse introduced me to GINA, the Global INitiative for Asthma. It was a phone consultation because the then new virus SARS-CoV-2, which causes what became known as COVID-19, was beginning to spread. At the time, I was very worried that it would be a killer for me given my asthma. Eventually, medical science learned that people with asthma were not necessarily at any greater risk of morbidity and mortality.
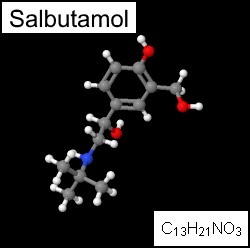
Anyway, it was nice to meet GINA. GINA contradicts some of what general practitioners (GPs) in the UK have been advising asthma patients for years, but supports what the medical evidence suggests one should do in terms of medication. The main thing is GINA told me to stop using Salbutamol (the reliever spray) and to use my Symbicort (combined preventer with reliever spray) instead. Salbutamol is an old, out-of-date drug with some unpleasant side effects in long-term use, partly because it can affect the heart but mainly because inappropriate use in the absence of proper control of the condition with a preventer can lead to scarring in the lungs.
Modern relievers are more targeted to the lungs rather than other organs. Moreover, using the preventer at a higher dose, which is what my nurse recommended, means you reduce inflammation and mucus production, which are the main issues with asthma in parallel with episodic bronchoconstriction.
For three years, I have been taking twice as much preventer each day as I was before, and only very occasionally need to take extra to get a dose of reliever. I have not used Salbutamol at all in those three years and don’t expect to have to ever again. I no longer carry Salbutamol with me.
A GP friend was concerned when I told him about GINA, he reasoned, quite sensibly that taking this approach would be increasing one’s exposure to the preventer drugs, which are corticosteroids. This is true. But asthma is mostly about inflammation and these drugs reduce inflammation and so should reduce asthma symptoms. They do. He discussed the issue with colleagues and is now persuaded that GINA is a more sensible approach to asthma control than the current NICE recommendations in the UK. Hopefully, someone will introduce NICE to GINA soon.




 Asthma sufferers, non-smokers, and those who really just don’t care for passive-smoking-induced lung cancer can breathe a long sigh of relief as England follows other enlightened states and places a ban on smoking in enclosed public places, such as pubs, clubs, and restaurants, from July 1, 2007.
Asthma sufferers, non-smokers, and those who really just don’t care for passive-smoking-induced lung cancer can breathe a long sigh of relief as England follows other enlightened states and places a ban on smoking in enclosed public places, such as pubs, clubs, and restaurants, from July 1, 2007.