A very different disease -Â David Bradley at the Royal Society, January 2004
The SARS epidemic of 2002-2003 was rather unusual, began Professor Roy Anderson FRS of the Department of Infectious Disease Epidemiology, at Imperial College London. For instance, its transmission efficiency was low by comparison with viruses such as Influenza A, it had a high case fatality rate especially amongst the elderly, and there was a high incidence of infection and among health workers.
In regions badly affected by SARS there was much suffering, many deaths, serious disruption to social and work activities, and considerable economic losses. The isolation and quarantining of hundreds of thousands of people became essential to bring the disease under control as too were the tight restrictions on travel in some countries. The World Health Organization also played a vital role in co-ordinating the international response and helping to bring the disease quickly under control. We were very lucky this time round, he said. Draconian public health measures are relatively simple to implement in China and other neighbouring regions where this particular disease originated, but how would the people of North America and Western Europe cope with such restrictions on their liberties as mass quarantining? The cause of SARS was narrowed down to a single coronavirus and diagnostic tests of varying precision have been developed to help us detect it. Epidemiological research must now be carried out to help us understand how the disease spreads, especially given what is actually a very low transmissibility of the virus, compared with influenza. Data capture and information capture systems were put in place somewhat late during the epidemic. In future outbreaks this area needs to be improved so that researchers can gather knowledge about the disease’s epidemiology. During the SARS epidemic data capture systems were more effective in some regions and entirely ineffective in others. An international, centralised database would also allow doctors to record the effects of different medicines on the disease and so provide useful information for other doctors an in the longer-term epidemiologists.
We were extremely lucky with the SARS epidemic, said Anderson. SARS caused a around 800 or so deaths, influenza type A kills 30000 people in the USA every year. In the next global epidemic, we may not be so lucky in terms of biology or where the disease emerges. He suggested that we must keep SARS in perspective but not become complacent and assume that “we have been successful once, we will be again”.
The emergence of SARS
Professor Nan Shan ZHONG of the Guangzhou Respiratory Disease Research Institute suggested in his talk that he would probably raise more questions than he would make conclusions. The first case of SARS in China was recorded on 25th November 2002, and he saw his first definite case in December. The subsequent outbreak of the disease caught the world’s health systems unprepared. The worst Chinese epidemic was in Beijing with 2500 cases, while Guangdong province, where SARS first emerged, had some 1500 cases. The result was serious impact on social stability, particularly in China, and ultimately on the global economy.
From both the clinical epidemiological and virological points of view, SARS originated in the Guangdong province of China. Data showed that there may have been interspecies transmission between wild animals and humans, explained ZHONG, and a national campaign to kill rats as one possible source of infection was instigated by the government. As ZHONG pointed out, while rats harbour many diseases it is other animals, in particular the palm civet, which has been demonstrated to be the host of the emergent virus. The virus was found to be highly concentrated in the civets’ faeces and the first cases in 2002 occurred among animal traders. ZHONG believes it imperative these animals are culled and their use in cuisine be stopped.
ZHONG suggests that the health authorities must remain alert for the possible resurgence of SARS during the winter of 2003-2004 and into the spring. Indeed, the Provincial Department of Health in Guangdong has formulated a pre-warning policy based on early identification based on antibody lab tests. With early reporting, early isolation must be enforced to allow the health services to manage a resurgence.
Professionals have now been trained to identify the disease quickly and accurately and a report network has been established throughout mainland China to ensure a rapid response to new SARS cases. ZHONG told the meeting that in the previous three weeks three new cases of SARS had emerged.
Should the disease re-emerge, corticosteroid and non-invasive ventilation should be reiterated as the treatment of choice for patients with critical SARS. Traditional Chinese medicine (TCM) may also have use in early adjunctive therapy. An inactivated SARS vaccine is now in clinical trials and early results suggest it is safe and efficacious and may be available in an emergency.
Fighting SARS in China
Victory over the first SARS epidemic resulted from the efforts of the medical and scientific communities and the political commitment of the authorities in China with strong international support; the causative agent having been identified within two weeks of the outbreak, said Professor CHEN Zhu Vice President of the Chinese Academy of Sciences (CAS). Two weeks later, the SARS genome was unravelled.
Three programmes have now been implemented under the Chinese taskforce – research into causes and effects, diagnosis, treatment and prevention, and drug and vaccine development.
The initial SARS infections, which were seen among restaurant researchers in particular, were rather weak, and reminiscent of the state of play at the time of the meeting in the advent of a SARS second coming. It was then the infamous “Super-Spreader” event in Guangzhou Second Hospital, which evoked the epidemics in Guangzhou, the second phase, and then the Hotel M event that ultimately led to the massive scale of the SARS epidemic, the third phase to Northern China and other countries/regions in the world. Comparisons of the genome at each phase together with information about the relation between human SARS and the disease in the animal carriers, palm civets, is providing important clues about controlling SARS and vaccine development.
With regard to diagnosis, treatment, and protection, CHEN added that Guangzhou’s Prof. ZHONG Nan Shan is something of a hero in China for having first identified SARS as a new pathogen; he and his collaborators developed effective treatments using corticosteroids, antiviral drugs and non-invasive positive pressure ventilation, as well as integrating it with Traditional Chinese Medicine.
Diagnostic tools and kits have been developed in response to the first epidemic are now revealing themselves to be critical in controlling the recent appearance of SARS cases in 2004. Physical protective equipment for personal and hospital use are also being rapidly developed, added CHEN. The Chinese government has issued new security guidelines to help it cope with another outbreak. The scientific conservation of samples of the SARS coronavirus for further researchers is another important measure that CHEN mentioned briefly.
Beijing researchers had reported at the time of the meeting the effectiveness of inactivated SARS viral particle in laboratory tests, but says CHEN , many questions remain to be answered before a safe and effective vaccine will be ready.
The lessons of SARS have led to open reporting, especially in China, which means “next time”, the international health and research communities will be better equipped to respond.
The victims of SARS
Robert Maunder’s hospital, the Mount Sinai Hospital in Toronto, was on the frontline during the SARS epidemic. One aspect of such an epidemic that does not always immediately come to mind is the psychological impact on health workers.
The outbreak of SARS in 2003 provided a system-wide stress upon healthcare workers in the Toronto region, said Maunder, reminding us of when public-health messages were common and quarantine widely used. To understand the psychological impact on hospital staff and the wider community, we should recall the eighteenth century when hospitals were considered places to die rather than centres of healing.
The disease hit Toronto in two waves, said maunder. The first wave had a major impact on Mount Sinai Hospital allowing the researchers to survey of healthcare workers at three hospitals in late May. The effect of stringent controls put in place meant no visitors and non-essential staff ordered to stay home. The public perception of hospitals was severely affected, hospitals were seen as places with disease, and healthcare workers were seen as victims and carriers of disease.
Maunder’s team has studied data from two sources of information. First, observations by he and his colleagues of administrators and mental health professionals providing support during the SARS epidemic in March and April, and a survey of about 1600 healthcare workers at three Toronto hospitals in May and June. The results provide a picture of the factors which lead the SARS outbreak to be experienced as a psychological trauma.
Maunder described how more than 35% of those surveyed reported severe stress symptoms, including intrusive thoughts and feelings and avoidance and blunted feelings. The degree of risk of traumatic stress was related to degree and duration of exposure to SARS patients as well as other factors. These included isolation from family and colleagues, and the wider community as well as job stress, and problems with family life. Rules prevented colleagues shaking hands or eating in the hospital cafeteria compound the problems leading to poor sleep, anxiety, and preoccupation with signs of illness among many healthcare workers.
There is a psychological cost to controlling a disease like SARS, said Maunder. This must be considered when planning the public-health response and invaluable psychological support provided during the early stages of an outbreak.
New hosts for new diseases
Biologist Dr Diana Bell of the University of East Anglia, Norwich, immediately drew three conclusions about the nature of emerging diseases like SARS.
First, she suggested that the search for diseases of animal origin should be extended, not only geographically, but also to small carnivores other than the masked palm civet from which SARS emerged. Secondly, there are major ecological shifts favouring the emergence of zoonotic diseases, in South East Asia. Thirdly, new collaboration between conservation biologists and vertebrate ecologists would help in finding and controlling such diseases.
The search for disease has focused on the animal markets of Southern China, but many of the animals traded here are illegally imported. The animal reservoir for SARS and other viruses could extend far outside China. Moreover, China’s neighbours in the Indochina hotspot of biodiversity – Cambodia, Laos, Thailand – also exploit wild animals in the restaurant trades, traditional medicine, perfumes, skins for clothing, and as pets. The limelight has shone on three small carnivore species: the masked palm civet, Chinese ferret badger, and raccoon dog. Many other endangered species are also exploited.
Bell suggested that putative hosts must be screened across all routes from capture to marketplace and beyond. This would allow researchers to pinpoint at what point the animals first show signs of infection.
Wildlife trade is a global problem, not restricted to South East Asia. African civets are eaten as bush meat and should be screened. Moreover, the problem is very much a global one. Huge numbers of wild animals are imported into the USA each year, including 49 million live amphibians and 2 million live reptiles. The wildlife trade, Bell said, is not only a threat to biodiversity but seriously threatens human health.
To combat this trade, it is important to hit supply and demand, said Bell. Better law enforcement and community participation as well as education could be key to reducing the demand for wild meat.
Read on in Session 4: Planning for disease

 “Food production occurs in several stages, each of which provides potential opportunities for bacterial contamination,” explains Johnson. He points out that generally chickens grown for commercial food production live in crowded conditions that are ideal for the spread of bacteria. While thorough cooking will kill most pathogenic bacteria that worm their way around food industry safety measures pre-cooked foods can easily be contaminated between cooking and final packaging steps.
“Food production occurs in several stages, each of which provides potential opportunities for bacterial contamination,” explains Johnson. He points out that generally chickens grown for commercial food production live in crowded conditions that are ideal for the spread of bacteria. While thorough cooking will kill most pathogenic bacteria that worm their way around food industry safety measures pre-cooked foods can easily be contaminated between cooking and final packaging steps.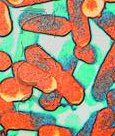 For Johnson and other food scientists, food safety is a matter of minimizing risks as much as possible, risks that will never completely go away. Pathogenic bacteria, he says, are tiny but formidable adversaries. There were some 65,209 food-poisoning cases in the UK not picked up while abroad in 2000. The Food Standards Agency wants to take Salmonella, E. coli O157, and Listeria monocytogenes off the menu wherever possible. Johnson told us that, “The zein-nisin coating will only work when cold refrigeration temperatures of 4 Celsius are used and only low numbers of the pathogen Listeria monocytogenes are encountered, say about 1,000 per gram. This strategy will not work for temperature-abused foods left out at room temperature.” Now, where’s that tarragon and lemon dressing?
For Johnson and other food scientists, food safety is a matter of minimizing risks as much as possible, risks that will never completely go away. Pathogenic bacteria, he says, are tiny but formidable adversaries. There were some 65,209 food-poisoning cases in the UK not picked up while abroad in 2000. The Food Standards Agency wants to take Salmonella, E. coli O157, and Listeria monocytogenes off the menu wherever possible. Johnson told us that, “The zein-nisin coating will only work when cold refrigeration temperatures of 4 Celsius are used and only low numbers of the pathogen Listeria monocytogenes are encountered, say about 1,000 per gram. This strategy will not work for temperature-abused foods left out at room temperature.” Now, where’s that tarragon and lemon dressing?